By Ross Pelton, RPh, PhD, CCN
Scientific Director, Essential Formulas
According to the World Health Organization (WHO), depression is now the most common illness and the leading cause of disability globally, affecting hundreds of millions of people.i Although depression can be caused by a wide range of conditions or situations, this article’s purpose is to report on emerging evidence, which indicates that antibiotics, which are known to disrupt the gut microbiome, increase the risk of a person becoming depressed.ii
In addition to depression, the widespread use of antibiotics in agricultural animals and the overprescribing of antibiotics by physicians are responsible for the rapid rise of antibiotic-resistant ‘superbug’ infections. This health crisis has been referred to as a “global threat” to humanity.iii
Antibiotics & Depression: In a review of antibiotics, depression, and the gut microbiome, it was reported that disruption of the gut microbiome plays a vital role in the development of depression.iv The mechanisms of communication between intestinal bacteria and the brain include the vagus nerve, gut hormone signaling, the immune system, or by way of postbiotic metabolites such as the amino acid tryptophan and short-chain fatty acids. Although the relationship between the microbiome/gut-brain communication is still unraveling, mounting evidence links disruption of the microbiome with risk for depression.v
It has been reported that the use of antibiotics during pregnancy increases the risk of postpartum depression.vi Results from an analysis of 97,680 pregnancies revealed that antibiotics are the most common class of medications prescribed to women 1-year before becoming pregnant, during pregnancy and after pregnancy.vii Approximately 43% of women took antibiotics 1-year before pregnancy, 26% of women took antibiotics during pregnancy, and 44% took antibiotics 1-year following pregnancy.
Antibiotics & Obesity: The widespread use of antibiotics may also be contributing to the epidemic of obesity. Strong evidence from animal studies has documented the role of antibiotics play in the disruption of the gut microbiome and the development of obesity.viii
Children born to mothers who take antibiotics during pregnancy are at a much higher risk of childhood obesity. In this study, 436, mother-child pairs were followed closely until the child reached the age of 7. Compared to children born to mothers who were not exposed to antibiotics during the second or third trimester, children exposed to antibiotics in utero had an 84% higher risk of becoming obese.ix Also, the antibiotic-obesity effect starts early in life, as evidenced by the fact that mothers who take antibiotics during pregnancy give birth to infants who have higher birth weights compared to women who were not given antibiotics.x
Antibiotics & Childhood Obesity: It has been well documented that administering antibiotics to children before they are two years old increases the risk of childhood obesity. Furthermore, childhood obesity frequently progresses to obesity in adulthood and increases the risk of diabetes, hypertension, and various forms of cancer.xi,xii It is estimated that one-third of children and adolescents in the United States are either overweight or obese.xiii Sadly, childhood obesity is now playing a significant role in the global obesity pandemic.
Obesity & Depression: There is a clear association between obesity and depression. A meta-analysis of 9 studies with a total of 171,701 individuals reported that obese individuals have a 32% increased risk of depression compared to healthy weight individuals.xiv
Antibiotics, the Microbiome, Depression & Obesity: Antibiotics cause significant disruption of the microbiome. In this article, I have summarized clinical trials, which report that antibiotic-induced Dysbiosis increases the risk of both depression and obesity.
A “Healthy” Microbiome: There is no agreed-upon definition of a “healthy microbiome, partly because each individual has their own unique and personal microbiome. Many variables can influence the composition of an individual’s microbiome. However, generalization is often proposed because a healthy gut microbiome contains a ratio of approximately 85%-90% beneficial probiotic bacteria, and only 10-15% harmful bacteria. Everyone’s microbiome contains some bad bacteria, but when good bacteria predominate, the harmful bacteria are held in check and do not present a problem.
Dysbiosis is a term that denotes an unbalanced microbiome. In addition to unpleasant gastrointestinal symptoms such as gas, bloating, and diarrhea, Dysbiosis can cause intestinal disorders such as irritable bowel syndrome (IBS), celiac disease, and allergies, asthma, metabolic syndrome, cardiovascular disease, obesity, and autoimmune diseases.xv Many factors can contribute to Dysbiosis, such as lack of dietary fiber, alcohol, sedentary lifestyle, environmental toxins, stress, and dehydration, to name a few. However, taking antibiotics is probably the fastest method of causing severe disruption to the microbiome.
Repairing or Improving the Microbiome: A healthy microbiome is essential for good health. Conversely, an unbalanced microbiome is associated with a wide range of diseases. Hence, it is crucial to rebuild a healthy microbiome following a course of antibiotics. However, many physicians and dentists do not provide instructions about probiotics or microbiome repair when prescribing antibiotics for their patients. Also, many people believe that just taking probiotics will “fix” their microbiome. Dietary fiber is the “food” for your probiotic bacteria. If you do not consume a fiber-rich diet, your probiotic bacteria will not thrive and survive.
Postbiotic Metabolites: The primary “job” of probiotic bacteria is to ferment dietary fibers, which results in the production of compounds referred to as postbiotic metabolites. There is a growing awareness that various types of postbiotic metabolites play essential roles in regulating many aspects of human health. This field of research is so exciting that postbiotic metabolites are referred to as the new frontier in microbiome research.xvi
Probiotics vs. Postbiotic Metabolites: There is a growing realization that directly ingesting postbiotic metabolites can elicit improvement in the gut microbiome much faster than taking a commercial product that contains just contains probiotic bacteria. When probiotic bacteria are ingested, they must survive transit through the harsh stomach acid. When they arrive in the intestinal tract, they must then begin the process of fermenting dietary fibers into postbiotic metabolites. This process takes time. When postbiotic metabolites are directly ingested, they immediately start to exert their health-regulating effects such as reducing inflammation, enhancing digestion, nutrient absorption, detoxification, immune function, gut-brain communication, and much more. Directly ingesting postbiotic metabolites promotes rapid improvements in the gut microbiome.xvii
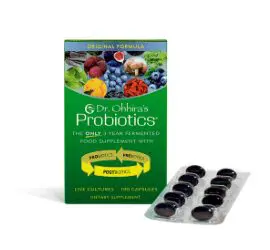
Dr. Ohhira’s Probiotics® is a fermented food probiotic that contains over 500 postbiotic metabolites. In this production process, 12 carefully selected strains of probiotic bacteria are added to sizeable 80-gallon fermentation vats along with dozens of organically grown, fiber-rich foods. The bacteria then ferment the fibers for three years (Original Formula) to 5 years (Professional Formula). The final product contains live probiotic bacteria, prebiotics, and, most importantly, over 500 postbiotic metabolites. This explains why Dr. Ohhira’s Probiotics have garnered a world-wide reputation for delivering fast improvements in the microbiome ecosystem. That’s ‘The Dr. Ohhira’s Difference.’
Br J Clin Pharmacol, 55 (2003), pp. 216-221